Accessible design focuses on creating inclusive technology that meets the needs of diverse users. In healthcare, integrating accessibility into Electronic Health Record (EHR) software is transforming clinical care across all fields, especially behavioral health. EHR systems that adhere to universal design principles streamline patient care and empower both practitioners and patients.
The Evolution of EHR Software in Behavioral Health
Historically, Electronic Health Record systems posed various challenges for behavioral health practitioners and patients, hampering care delivery and engagement.
EHR interfaces were often complex and cluttered, with poor navigational design that made clinical documentation tedious and error-prone. Limited customizability also prevented the optimization of software workflows to match clinical needs and terminology. This inhibited practicing evidence-based care.
For patients, inaccessible portals and care plans prevented active participation in care. Difficulty accessing and comprehending records due to poor interface design reduced transparency and shared decision-making.
However, the disability rights movement and legislation like the Americans with Disabilities Act led to greater recognition of the rights and needs of people with disabilities. This drove increased prioritization of accessible, patient-centered design in health information technology.
As a result, modern EHR software for behavioral health and other medical fields are increasingly designed incorporating principles of universal accessibility and usability. Customization options allow better tailoring software to support unique clinical workflows and documentation needs in behavioral health settings. Intuitive interfaces facilitate usage for diverse patients and practitioners.
These ongoing advances are closing critical gaps in EHR design that previously hindered the delivery of integrated, comprehensive care. Thoughtfully designed, accessible EHRs are optimizing clinician workflows while enhancing transparency and the care experience for patients.
Key Accessibility Features in Modern EHR Software
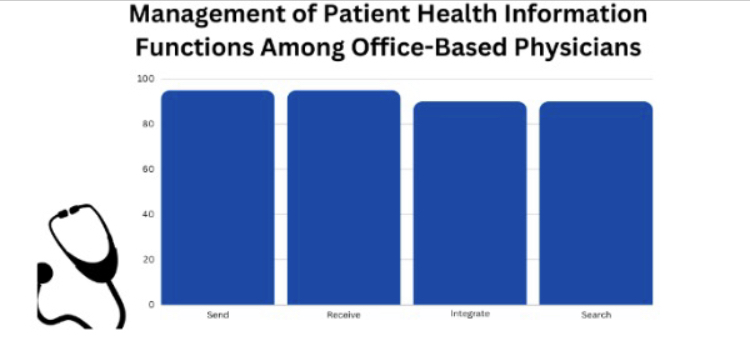
Source: Center of Disease and Control
In the realm of modern EHR software, prioritizing accessibility has become a cornerstone of design, with numerous features tailored to enhance usability for diverse users. Modern EHR systems incorporate various features focused on improving accessibility and usability for diverse users.
Simple, consistent navigation and interface design provides intuitive, seamless usage for all users. Keyboard shortcuts, voice commands, and screen reader integration assist those with mobility or visual disabilities. Customizable text sizing aids those with visual impairments.
Highly configurable documentation tools allow clinicians to closely model patient records after clinical needs. Templates, diagrams, drawings, and multimedia attachments add richness to notes. Shared templates boost interdisciplinary coordination and standardization.
Patient portals are readable and understandable to those with varying literacy levels. Integrated education aids increase health literacy. Secure messaging enables direct engagement. Accessibility testing ensures portal usability for diverse patients.
Cross-platform accessibility enables the use of EHRs on various devices and operating systems. As technology evolves, maintaining accessibility across platforms will be key.
Enhancing Patient Care with Accessible EHRs
Thoughtfully designed, accessible EHRs with extensive patient testing confer several advantages to enhance patient care quality in behavioral health settings.
Streamlined, user-friendly interfaces help clinicians accurately and completely record health data. Customization also aids in collecting pertinent psychosocial history and structuring progress notes tailored to care. This facilitates delivering holistic, patient-centered care.
Data interoperability with healthcare partners is also improved with accessible EHRs. Secure sharing of comprehensive health records with primary care providers and health systems enhances care coordination and outcomes.
For patients, accessible portals allow direct, secure access to their records. This promotes transparency, engagement, and shared decision-making. Accessible design ensures patients of diverse needs can fully utilize these tools.
The Future of Accessibility in Behavioral Health EHRs
Innovations in natural language processing, predictive analytics, and artificial intelligence hold promise for enhancing accessibility further. Voice-enabled documentation and intelligent data analysis can reduce clinician workload and errors. Chatbots and virtual assistants can improve patient engagement.
However, there is still work to be done in spreading accessibility-focused design practices across the industry and promoting inclusion. Health information technology vendors must uphold accessibility as a key tenet and actively solicit user feedback. Provider organizations should demand inclusive products during system selection and configuration.
Through sustained collaborative efforts, EHR systems can fulfill the promise of streamlined, patient-centered care in behavioral health and beyond. Accessible design principles will be pivotal in unlocking the full potential of health information technology.
The ongoing integration of accessible design principles, combined with advancements in analytics, holds the promise of delivering streamlined, patient-centered care and optimizing the overall healthcare experience.
Frequently Asked Questions (FAQs)
How does accessible EHR software benefit patients with behavioral health issues?
Accessible portals allow patients to conveniently access records, improving transparency. Customization also helps capture patient needs accurately. This facilitates patient-centered treatment plans.
Are there legal requirements for EHR accessibility in behavioral health?
Yes, the Americans with Disabilities Act and Section 508 standards require EHR accessibility to those with disabilities. Healthcare organizations must provide accessible health records.
What challenges do healthcare providers encounter when implementing accessible EHR systems?
Overcoming entrenched workflows and change resistance is common. Adequate staff training and leveraging external accessibility expertise ease the transition. Gradual rollout also allows adapting to new systems.
In summary, incorporating accessible design principles in EHR systems delivers tremendous potential to transform care delivery in behavioral health. Continued focus on inclusive, user-centric design will be the key to unlocking the full promise of health information technology.
Final Takeaway
The historical complexity and poor navigational design of EHR systems posed obstacles for behavioral health practitioners, hindering efficient care delivery and evidence-based practices. Patients faced barriers to active participation due to inaccessible portals and care plans, impacting transparency and shared decision-making.
However, recognizing the rights and needs of people with disabilities, coupled with legislation like the Americans with Disabilities Act, paved the way for prioritizing accessible, patient-centered design in health information technology. Modern EHR systems now embrace customization options, intuitive interfaces, and universal accessibility features that address the unique needs of diverse users.
Looking ahead, the future of accessible EHRs in behavioral health holds promising innovations, including natural language processing, predictive analytics, and artificial intelligence. These advancements have the potential to further reduce clinician workload, enhance patient engagement, and improve overall care outcomes.
This evolution in technology is not only about improving the functionalities of EHR systems but also about enhancing the overall healthcare experience for both providers and patients. The trajectory of accessible EHRs underscores a commitment to inclusivity, efficiency, and continuous improvement. As the industry collectively embraces these advancements, the future landscape of behavioral health EHRs holds the promise of being more accessible, intelligent, and patient-centered than ever before.


